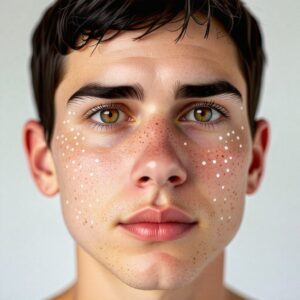
Everything You Need to Know About Vitiligo: Causes, Symptoms, and Treatment Options
Vitiligo is a condition that causes patches of skin to lose their pigment, resulting in lighter areas that can develop anywhere on the body. While it is not a life-threatening condition, it can have profound effects on an individual’s emotional and social well-being. This article aims to explore the causes, symptoms, and most effective treatment options for vitiligo, answering common questions that many people have about the condition. Whether you’re recently diagnosed or simply curious, this guide will provide essential information on how to manage and treat vitiligo.
What is Vitiligo?
Vitiligo is a skin disorder that leads to the gradual loss of pigment in certain areas of the skin. The condition occurs when melanocytes, the cells responsible for producing melanin (the pigment that gives skin its color), are destroyed or no longer function. The result is the development of white patches that contrast with the surrounding skin. While these patches can appear anywhere on the body, they are most common on areas that are frequently exposed to sunlight, such as the face, hands, arms, and feet.
Though vitiligo is not contagious and does not directly affect physical health, it can be emotionally distressing for many people. The unpredictability of the condition, along with the visible nature of the patches, often leads to feelings of self-consciousness and anxiety.
What Causes Vitiligo?
While scientists are still studying the exact cause of vitiligo, a few factors have been identified as likely contributors:
1. Autoimmune Response
One of the most widely accepted theories is that vitiligo is an autoimmune disorder. In people with vitiligo, the body’s immune system mistakenly attacks and destroys its own melanocytes. This leads to the loss of pigment-producing cells and the appearance of white patches on the skin.
2. Genetics and Family History
Vitiligo often runs in families, which suggests a genetic component to the condition. People with a family history of vitiligo or other autoimmune disorders are more likely to develop it themselves. Specific genes related to immune function have been associated with an increased risk of vitiligo.
3. Environmental Triggers
Stress, physical injury to the skin, or sunburn may trigger or worsen vitiligo in individuals who are genetically predisposed to the condition. For example, sunburn can cause damage to melanocytes, and in people with a genetic susceptibility, this can lead to the development of vitiligo.
4. Hormonal Changes
Hormonal changes, such as those experienced during pregnancy, puberty, or menopause, may also play a role in the onset or progression of vitiligo. This might explain why vitiligo sometimes begins during these life stages.
Common Symptoms of Vitiligo
The primary symptom of vitiligo is the appearance of white or light patches of skin. These patches may first appear as small spots that gradually increase in size. Over time, they can spread to different areas of the body. Vitiligo patches are most commonly found on sun-exposed areas, such as:
- Face
- Hands and arms
- Neck
- Feet and legs
Other symptoms include:
- Premature graying of hair: Hair on areas affected by vitiligo may turn white or gray, as the melanocytes in the hair follicles are also destroyed.
- Increased sensitivity to the sun: Depigmented skin is more vulnerable to UV rays, making it more likely to burn.
Types of Vitiligo
There are two primary types of vitiligo:
1. Non-Segmental Vitiligo
This is the most common form of vitiligo, characterized by symmetrical depigmented patches that appear on both sides of the body. It usually progresses slowly and affects multiple areas. It can be widespread, with patches appearing on the face, hands, and other areas.
2. Segmental Vitiligo
Segmental vitiligo is less common and tends to affect only one side of the body. It can develop quickly and spread rapidly at first, but it typically stabilizes after a certain period. The patches often appear in a more localized area, such as one side of the face or hands.
How is Vitiligo Diagnosed?
If you notice white patches on your skin, it’s important to consult with a dermatologist. The diagnosis of vitiligo is typically made based on a visual examination and a review of your medical history. In some cases, additional tests such as a skin biopsy or blood tests may be done to rule out other conditions that can cause similar symptoms, such as fungal infections or leprosy.
In certain cases, a Wood’s lamp (a special ultraviolet light) may be used to help the doctor assess the extent of the pigmentation loss.
Treatment Options for Vitiligo
Although there is no known cure for vitiligo, there are various treatments that can help restore pigment to the skin or camouflage the patches. Treatment effectiveness can vary from person to person, and often a combination of methods is needed.
1. Topical Corticosteroids
Corticosteroid creams or ointments are commonly prescribed to reduce inflammation and suppress the immune response attacking melanocytes. These treatments can help repigment the skin, especially in the early stages of the condition. However, long-term use of these creams may have side effects, such as thinning skin.
2. Narrowband UVB Phototherapy
Phototherapy involves exposing the skin to ultraviolet (UV) light in a controlled environment. Narrowband UVB light is the most commonly used treatment for vitiligo. It stimulates the melanocytes to produce melanin, helping to restore pigment in affected areas. Phototherapy is often done several times a week under the supervision of a dermatologist.
3. Topical Calcineurin Inhibitors
Medications like tacrolimus and pimecrolimus can be used as alternatives to steroids, especially for sensitive areas like the face and genital region. These treatments help suppress the immune system and can promote repigmentation without the side effects of steroids.
4. Skin Grafting and Micropigmentation
For more severe cases of vitiligo, surgical options such as skin grafting (transplanting pigmented skin from one area to another) or micropigmentation (a type of tattooing) can be used to cover depigmented patches. These techniques are usually considered when other treatments have failed.
5. Depigmentation
For widespread vitiligo, depigmentation therapy may be an option. This involves lightening the remaining pigmented areas of the skin using chemical agents so that the entire skin becomes uniformly pale. This is a permanent solution, but it is generally only recommended for those with extensive vitiligo.
Managing Vitiligo with Lifestyle Changes
In addition to medical treatments, lifestyle adjustments can help manage the condition:
- Sun Protection: People with vitiligo need to be extra cautious about sun exposure. Sunscreens with a high SPF should be applied to depigmented areas to protect them from UV damage and sunburn.
- Cosmetic Camouflage: Using makeup or self-tanning products can help conceal white patches and boost self-confidence.
- Healthy Diet and Stress Management: While diet and stress do not directly impact vitiligo, maintaining a healthy lifestyle can improve overall well-being and emotional health, which can help cope with the psychological effects of the condition.
The Psychological Impact of Vitiligo
Vitiligo can be emotionally challenging, particularly when it affects visible areas like the face. People may experience anxiety, depression, or self-esteem issues due to their appearance. It’s crucial for individuals with vitiligo to seek emotional support from mental health professionals, support groups, or friends and family who understand the challenges of living with the condition.
Conclusion: Living with Vitiligo
While vitiligo can be a challenging condition, it’s important to remember that it does not define a person’s worth or abilities. With the right treatment and emotional support, individuals with vitiligo can lead happy and fulfilling lives. If you notice signs of vitiligo, consult with a dermatologist to explore your treatment options. Remember, you’re not alone in this journey – there are numerous resources available to help you manage both the physical and emotional aspects of vitiligo.